When a strep infection ends with an autoimmune hepatitis diagnosis
A few weeks ago my 3 year old nephew, Ryder, went through an incredibly scary health scare that came out of no where. Today, my sister and her husband, Jeff, are sharing their experience.
Jeff and I have wanted to write this post for a while, but weren’t sure how to start. These past few weeks have been some of the most stressful and emotionally draining of our lives. It started with a strep infection (which wasn’t our first) and ended with an autoimmune hepatitis diagnosis. Here’s our story:
Meet Ryder
Ryder is your typical high-energy, occasionally crazy, fun-loving 3 year old. He loves ninja turtles, mac and cheese and hates napping. Besides the occasional ear infection or cold, Ryder hasn’t had any health issues since he was born.

How it all started
It started a few weeks back when Ryder had a strep infection. It wasn’t his first and nothing seemed out of the ordinary until a few days later his skin was visibly yellow. His pediatrician drew blood to check his liver enzymes and sent us home. The next day I received a call that will haunt me forever. It was our pediatrician telling us to go to the emergency room immediately because Ryder was in active liver failure. We found out later that his aspartate transaminase (AST) was 1343 (normal range 3-34), alanine transaminase (ALT) was 3995 (normal range 15-41) and bilirubin was 8.4 (normal range 0.2-1.3). Even if you don’t know what any of those are, which we didn’t at the time, you knew it wasn’t good. Keep in mind I’m not a doctor and am just describing our experience, but these were the three liver enzymes we tracked closely.
At the Emergency Room
At the ER, the doctors drew blood to check Ryder’s liver function. A few hours later they informed us that Ryder’s liver numbers were rising and they were transferring him by ambulance to Georgetown Children’s hospital where they would be better equipped to handle his case. At that point we had been in the ER for about 6 hours and it would still be another 3 hours before an ambulance would be available. Considering the situation, Ryder did really well. For us, on the other hand, it took everything we had to keep it together.

At Georgetown Pediatric Hospital
At Georgetown, the doctors took vial after vial of blood. They explained that when someone goes into acute liver failure, the most important thing is to figure out the cause. In the meantime, Ryder was given IV IgG and IV antibiotics. The IV antibiotics were to fight off any potential bacterial infection. The IV IgG was to boost his immune system so it could mount a more robust response against any other type of infection. He got 2 IV IgG treatments, each taking 4 hours to administer.
Most of the poking and probing happened the second day and it was tough on Ryder. Our hearts broke a little each time they had to draw more blood. Our doctor explained that in addition to blood work, Ryder would also have a fine needle liver biopsy, a bone marrow biopsy and a liver ultrasound. If there was ever a time to bribe your child, now was it. We let Ryder scroll through toy options on amazon and pick out 1, 2 or 10 (or more, not sure). Truth be told, he could have asked for anything and we would have ordered it without hesitation.
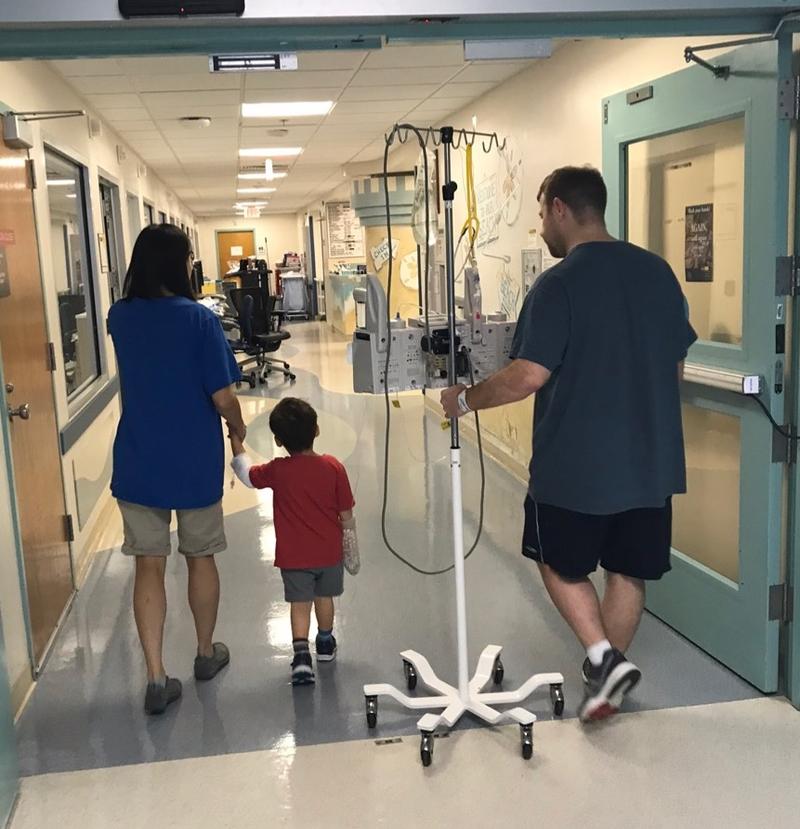
By the third day things were calmer and we were finally able to take a breath and Ryder was able to leave his room (and take showers!). Anything the doctor said to us before that point was a blur of information. The doctor explained that there is some research that shows a strep infection can “wake up” the Epstein-Barr virus (EBV), which can trigger the onset of autoimmune hepatitis. She also explained they don’t know why it happens to some people, and it is most likely a combination of being genetically predisposed and environmental factors.
Side note: *A genetic predisposition just means you have inherited certain genetic variants from your parents that increase your likelihood for developing a particular condition. However, since most condition are influenced by your environment as well as your genetics, a predisposition does not necessarily mean you will develop the trait._
Liver and bone marrow biopsies
The plan was to sedate Ryder for the biopsies. Ryder had been in the hospital for several days and was ready to go home. He was tired of being stuck with needles and there was no way he was going to willingly let anything be biopsied. The liver biopsy would tell us if there was any damage to his liver given how high his liver enzymes got. The bone marrow biopsy was to determine why his white blood cell count got so low. The good news is his liver and bone marrow biopsies came out clean - meaning no damage to his liver had occurred. The other good news at this point was that his liver enzymes were trending down. They were still extremely high, but they weren’t getting worse.
Diagnosis - Autoimmune hepatitis (AIH)
When the doctor first said the words “autoimmune hepatitis”, we immediately thought hepatitis A, B or C. But autoimmune hepatitis is completely unrelated and simply means Ryder’s immune system is attacking his liver. And your immune system isn’t suppose to do that. Our doctor referred us to this site to get more information on AIH.
Managing the diagnosis
Once we got the diagnosis, our attention shifted to how to manage/treat Ryder’s condition. Unfortunately AIH isn’t something that can be cured, but if caught early and monitored properly it also isn’t a debilitating condition. If his treatment is successful he may never have another “liver failure” incident again. The initial plan was to treat with a corticosteroid, Prednisone, until his liver levels returned to normal, then switch to a low dose immunosuppressant. In a nutshell, Ryder’s immune system is activating his immune cells to attack his liver. If left untreated, the condition can potentially progress to cirrhosis and end-stage liver failure. To avoid that, Ryder will take a low dose immunosuppressant. The idea is to dampen his immune response so it won’t attack his liver again.
Before we were discharged from the hospital, we met with a lifestyle coach. Georgetown has amazing pediatric lifestyle coaches who are there to help transition little ones to a new medical norm. In our case, the lifestyle coach helped us figure out the best way to give meds to Ryder. If any of you have 3 year olds, you know that this is not an easy task. Most kids his age do best with a liquid form, but Ryder refused. The lifestyle coach was incredibly patient and figured out a way to get Ryder to swallow pills. I’m still in awe of how she managed that, but she did and to this day he still takes his pills. In fact, Ryder’s childlife coach told us that to date, Ryder is the youngest child she has ever coached through pill swallowing–needless to say this was a proud parent moment.
Leaving the hospital
When we left the hospital, Ryder’s liver enzymes were still very high. But because they were trending down, his doctor felt comfortable monitoring Ryder as an out patient. It took a few more weeks but his liver enzymes finally got back to normal! Now we are slowly weaning him off the prednisone. His liver enzymes are checked every 2 weeks. If his levels remain normal, we reduce his Prednisone dose by 1 mg. Once he is completely off the Prednisone we will start giving him the low dose immunosuppressant.
Overall, this experience has been hard, but we are so thankful for the amazing doctors and nurses who cared for Ryder. And we are so thankful for the amazing support we have received from friends and family. Your support has been more appreciated than you know. Thank you.
We are still learning about AIH, but if you’d like to know more visit the Center for Autoimmune Liver Disease via Cincinnati Children’s Hospital.